Adapting American Heart Association Guidelines to the South African Context
Adapting American Heart Association Guidelines to the South African Context
DISCLAIMER
This blog contains discussions and general information about medical emergencies and other health topics. The information in this blog and in other related resources is not meant to be medical advice, and it should not be taken as such. The information contained in this blog should not be used in place of a medical doctor’s advice or treatment. If you or someone else has a medical concern, you should talk to your doctor or seek out other professional medical care. The opinions and views on this blog and website have no connection to those of any school, hospital, medical facility, or other organization.
Implementing the American Heart Association (AHA) guidelines in South Africa offers an opportunity to enhance cardiovascular care across the nation. These guidelines provide a robust framework for managing cardiac emergencies. But, adapting them to the South African context requires addressing unique local challenges and leveraging existing strengths. In this blog post, we will explore the various facets of this adaptation process by examining the “Chain of Survival”.
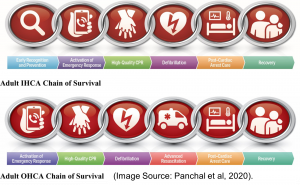
What is the Chain of Survival?
The American Heart Association chain of survival comprises six domains of care that ought to seamlessly integrate:
- Recognition of cardiac arrest and activation of the emergency response system,
- Early cardiopulmonary resuscitation (CPR),
- Rapid defibrillation,
- Advanced resuscitation by Emergency Medical Services (EMS) and other healthcare providers,
- Post-cardiac arrest care,
- And recovery (including rehabilitation).
Recognition of Cardiac Arrest and Activation of the Emergency Response System
Understanding The American Heart Association Guidelines
The American Heart Association (AHA) guidelines are a cornerstone of cardiovascular and Stroke care, providing comprehensive protocols for managing Medical emergencies. These guidelines cover adult and paediatric basic and advanced life support, neonatal resuscitation, and first aid. The 2020 updates highlight several critical components:
- Recognition and Activation: Identifying cardiac arrest quickly and activating the emergency response system is crucial. Immediate recognition leads to prompt action, increasing the chances of survival.
- High-Quality CPR: Emphasizing the importance of effective chest compressions, the guidelines specify the depth and rate of compressions to maximize the chances of survival (Panchal et al, 2020).
- Rapid Defibrillation: Using automated external defibrillators (AEDs) as soon as possible to treat life-threatening arrhythmias is essential to improve outcomes.
- Integrated Post-Cardiac Arrest Care: After achieving return of spontaneous circulation (ROSC), comprehensive care, including targeted temperature management and neurological support, enhances recovery and long-term survival (Merchant et al., 2020).
- Continuous Evidence Evaluation: Regular updates based on the latest scientific evidence ensure that healthcare providers are equipped with the most current and effective strategies for managing cardiac emergencies.
By understanding and implementing these guidelines effectively, healthcare providers in South Africa can significantly enhance the quality of care and survival rates for cardiac arrest patients.
Challenges in the South African Context
Emergency Medical Services (EMS) Dispatch System
South Africa’s EMS dispatch system faces significant challenges that impede the success of CPR and ECC protocols recommended by the AHA. Delayed response times, inefficient dispatch systems, and logistical hurdles are critical issues.
A recent study on telephonic descriptions of out-of-hospital cardiac arrest (OHCA) by laypersons calling the dispatch center of a private EMS in South Africa highlights some of these challenges. The study found that call-takers rely heavily on the descriptions provided by callers to identify OHCA, which can be problematic if the caller is unable to accurately describe the patient’s condition (Crause et al., 2023). Keywords and phrases used by callers to describe OHCA were organized into five categories: cardiac activity, level of consciousness, breathing descriptors, ill health, and clinical features. The most common descriptors related to suspected death and unresponsiveness, which aligns with findings from previous studies in the Western Cape (Crause et al., 2023).
The study also noted that call-takers often face difficulties in accurately triaging calls due to incomplete or unclear information provided by callers. This issue is compounded by the fact that many call-takers lack formal healthcare credentials and rely on home-grown dispatch methods, leading to inconsistencies in triage decisions (Crause et al., 2023). Additionally, call-takers must manage the tension between accurately triaging calls and the legal risks associated with under-triage, often leading to a preference for over-triage (Crause et al., 2023).
Participants in focus groups from the Western Cape Government EMS system identified several key areas for improvement to increase dispatch effectiveness, including:
- Time Constraints: The urgency of dispatching calls within strict timeframes often leads to initial misclassification of priority levels.
- Communication: Tensions between call takers/dispatchers and EMS crews, particularly when crews arrive at scenes to find non-critical patients.
- Legal Risks: The preference for over-triage due to fear of legal consequences if a patient’s condition is underestimated.
- Incoming Calls: Issues with inaccurate or incomplete information from callers, often leading to misclassification.
- System Constraints: Understaffing and a fixed number of vehicles limit the system’s capacity to handle emergencies effectively.
- Complaint Categorization: The need for better-defined categories and guidelines to assist call takers in making accurate triage decisions (Alshehri et al., 2020).
To address these Challenges the following strategies, should be considered:
Implementation of Computer-Aided Dispatch Systems
The South Africa National Health Act, 2003, and the 2022 Regulations relating to the Standards for Emergency Medical Services, emphasize the need for a Computer-Aided Dispatch (CAD) system to facilitate vehicle allocation, routing, and tracking. In cases where an Emergency Communication Centre (ECC) does not have a CAD system, a paper-based system must be utilized to ensure vehicle allocation, direction, and tracking (Regulations relating to the Standards for Emergency Medical Services,2022). The integration of CAD systems can significantly enhance the efficiency of EMS dispatch by providing real-time tracking of emergency vehicles and optimizing their allocation based on location and availability. This technology enables quicker response times, which is crucial for improving survival rates during cardiac arrest and other emergencies (Kurz et al., 2020).
Standardized Dispatch Processes and Monitoring
Establishing standardized processes for dispatching vehicles is another critical step in upgrading EMS dispatch systems. Standardization ensures consistency and reliability in the dispatch process, reducing the chances of errors and delays. The regulations mandate that the EMS must monitor response times for each stage of the call management and dispatch process to identify areas needing improvement and ensure timely interventions (Regulations relating to the Standards for Emergency Medical Services, 2022).
Regular monitoring and quality improvement initiatives are essential to maintaining high standards in EMS dispatch operations. By analysing response times and other performance metrics, EMS agencies can continuously refine their processes and implement best practices to enhance overall efficiency and effectiveness (Kurz et al, 2020).
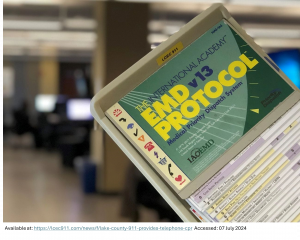
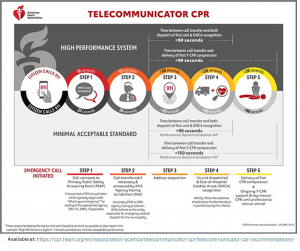
Telecommunicator CPR (T-CPR) Implementation
Telecommunicator CPR (T-CPR) is a vital component of the EMS dispatch system, as telecommunicators are the first responders who can guide callers through CPR procedures while waiting for EMS to arrive. The American Heart Association (AHA) recommends that all dispatch centres implement T-CPR programs, which include training telecommunicators to recognize cardiac arrest and provide CPR instructions over the phone (Kurz et al., 2020)
To implement T-CPR effectively, dispatch centres must commit to ongoing training and quality improvement measures. Initial training for call takers and dispatchers should be comprehensive, with regular continuing education to ensure skills are maintained and updated. Quality improvement audits should be conducted for all calls where resuscitation is attempted, collecting key time intervals and reasons for non-recognition or delays in providing T-CPR (Kurz et al, 2020)
Coordination with EMS Agencies
Close coordination between dispatch centres and various EMS providers is essential to ensure a seamless response to emergencies. Data linkage between dispatch audio records and EMS run reports allows for accurate tracking of cardiac arrest cases and performance measurement of the dispatch system. Having a designated medical director for the communications centre, ideally shared with the EMS agency, can enhance the implementation of T-CPR protocols and ensure consistent medical oversight (Kurz et al., 2020)
Resource Allocation
The allocation of medical resources in South Africa is uneven, with rural areas suffering the most from a lack of advanced medical equipment and trained personnel. This disparity hampers the effective implementation of AHA guidelines, which emphasize the importance of immediate and advanced care for cardiac emergencies. To bridge this gap, there must be a concerted effort to equip rural medical facilities with essential life-saving equipment, such as automated external defibrillators (AEDs) and advanced resuscitation tools. Additionally, increasing the number of trained EMS personnel in these areas through targeted recruitment and training programs can significantly improve emergency care delivery.
A report by the South African Human Rights Commission (SAHRC) on access to emergency medical services in the Eastern Cape (2015) highlighted significant issues related to resource allocation. The Eastern Cape Department of Health (ECDoH) has an insufficient number of ambulances and qualified emergency service personnel, with an even smaller number of operational ambulances available to respond to emergency situations. This shortage is further exacerbated by the lack of Planned Patient Transport and Inter-Facility Transport vehicles, which delays response times and limits access to emergency care (SAHRC, 2015).
The poor state of the road network, particularly in rural areas, further hinders the ability of ambulances to reach patients promptly. Many ambulances lack 4×4 capabilities, making it difficult to navigate challenging terrains, resulting in delays or an inability to respond to emergencies. Consequently, patients often resort to costly private transportation options, which can be financially devastating for families living in poverty (SAHRC, 2015).
A study conducted in the eThekwini district of KwaZulu-Natal highlighted the significant mismatch between the dispatch of EMS resources and actual patient needs, indicating high levels of inappropriate emergency responses. The study found that over 56% of cases dispatched as high-priority “red-code” emergencies only accounted for less than 2% at the scene, revealing an over-triage rate of over 93% (Newton et al., 2015). This inefficiency not only strains the EMS resources but also impacts the ability to respond effectively to genuine emergencies.
Moreover, the study reported that more than 58% of cases attended by EMS required no intervention or only transportation, with less than 36% requiring basic life support (BLS) intervention. Advanced life support (ALS) interventions were required in only 1.4% of cases, yet ALS resources were dispatched for patients who ultimately did not need such high levels of care. This highlights the overutilization of limited ALS resources, which could be better allocated to areas with genuine need (Newton et al., 2015).
The inefficiencies in resource allocation are further compounded by the lack of formal EMS dispatch systems and the reliance on emergency medical dispatchers who may not always accurately assess the level of response needed based on caller information. This results in the inappropriate use of EMS units and unnecessary costs, ultimately reducing the overall effectiveness of the EMS system.
Addressing these challenges requires the implementation of evidence-based dispatch systems such as the Medical Priority Dispatch System (MPDS), which uses standardized protocols and algorithmic interrogation processes to prioritize patients accurately. Additionally, alternative routing of patients, such as referring non-emergency cases to appropriate care facilities or providing on-scene treatment and discharge, can help optimize the use of limited EMS resources (Newton et al., 2015).
Early Cardiopulmonary Resuscitation (CPR)
CPR Training
The AHA emphasizes widespread CPR training among laypersons and healthcare providers to improve out-of-hospital cardiac arrest outcomes. However, access to CPR training programs in South Africa is limited. Public awareness campaigns can promote the importance of CPR training and encourage community participation. Schools, community centres, and workplaces can serve as venues for regular CPR training sessions. Implementing mandatory CPR training as part of the school curriculum can ensure young individuals are equipped with these critical life-saving skills from an early age (Veronese et al., 2018).
CPR Certification Programs
There is a pressing need for more accredited training centres in South Africa that offer AHA-compliant certification programs. Establishing these centres across various regions, especially in underserved areas, can enhance the accessibility of high-quality training. Collaboration with international organizations to adopt best practices can further strengthen the training infrastructure. Regular re-certification and continuous professional development are crucial to maintaining high standards of CPR performance (Veronese et al., 2018).
Rapid Defibrillation
Importance of AEDs
Rapid defibrillation is critical for treating life-threatening arrhythmias such as ventricular fibrillation and pulseless ventricular tachycardia. The AHA guidelines recommend the use of automated external defibrillators (AEDs) as soon as possible to improve outcomes. The availability of AEDs in public places and within EMS vehicles can significantly enhance the chances of survival during cardiac emergencies.
Implementation Challenges
In South Africa, the availability of AEDs is limited, particularly in rural and underserved areas. This shortage is compounded by the lack of public awareness and training on how to use AEDs. Addressing these challenges requires a concerted effort to increase the distribution of AEDs and to educate the public and healthcare providers on their use. Policies mandating the presence of AEDs in public spaces and workplaces can also contribute to more widespread availability and use.
Advanced Resuscitation by Emergency Medical Services (EMS) and Other Healthcare Providers
Advanced Resuscitation Techniques
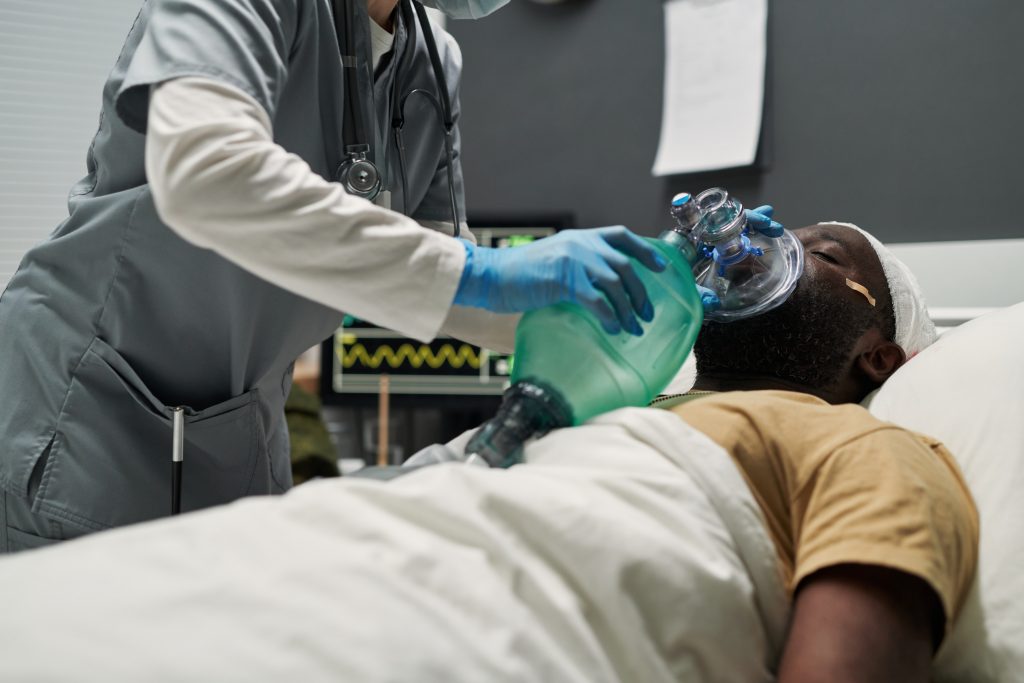
Advanced resuscitation involves the use of techniques such as administration of intravenous medications, and advanced airway management. These interventions are crucial for stabilizing patients during cardiac emergencies and improving their chances of survival. The AHA guidelines provide detailed protocols for these advanced interventions, which are essential for EMS personnel and other healthcare providers.
Training for EMS Personnel
Continuous professional development is essential for EMS personnel to stay updated on AHA guidelines and advanced life support techniques. Regular training sessions and workshops can enhance pre-hospital care, ensuring that EMS staff are well-prepared to handle cardiac emergencies effectively. This ongoing education can lead to improved patient outcomes and better alignment with international best practices.
Post-Cardiac Arrest Care
Integrated Post-Cardiac Arrest Care
After achieving return of spontaneous circulation (ROSC), comprehensive post-cardiac arrest care is vital for improving patient outcomes. The AHA guidelines emphasize hemodynamic optimization, targeted temperature management and neurological support as key components of post-cardiac arrest care. These interventions help stabilize patients, prevent complications, and enhance long-term survival.
Hospital Readiness
Many South African hospitals lack the necessary infrastructure to implement advanced post-cardiac arrest care, which includes therapeutic hypothermia and advanced life support measures. This shortfall is particularly evident in hospitals located in rural and economically disadvantaged areas. To adhere to AHA recommendations, it is essential to invest in hospital infrastructure upgrades. This includes equipping hospitals with advanced medical technology, creating dedicated cardiac arrest units, and ensuring the availability of essential medications and equipment (SAHRC, 2015).
Recovery and Rehabilitation
Recovery from cardiac arrest involves not only immediate medical care but also long-term rehabilitation. The AHA guidelines recommend a comprehensive approach to recovery that includes physical therapy, occupational therapy, and psychological support. These services are crucial for helping patients regain their independence and quality of life after a cardiac event.
Community Support and Follow-Up Care
Community support systems and follow-up care play a significant role in the recovery process. Regular follow-up appointments with healthcare providers, support groups, and educational programs can help patients manage their health and prevent future cardiac events. In South Africa, enhancing these support systems requires collaboration between healthcare providers, community organizations, and government agencies.
Conclusion
Adapting the AHA guidelines to the South African context requires a multifaceted approach that addresses the unique challenges faced by the country’s healthcare system. By enhancing EMS capabilities, promoting public CPR training, strengthening healthcare infrastructure, and advocating for supportive policies, South Africa can improve its cardiovascular care and patient outcomes. Collaboration between government, healthcare providers, and communities is essential to achieving these goals and ensuring that AHA recommendations are effectively implemented.
Health & Safety Training of Center South Africa (HSTCSA) – Emergency Care Education
The Health and Safety Training Center of South Africa, based in Pinetown, Durban, is renowned for its comprehensive life support training programs. Offering American Heart Association approved Basic Life Support and Advanced Cardiovascular Life Support courses, the center ensures participants receive high-quality instruction aligned with international standards.
Whether you’re looking for a basic life support course in Durban or an ACLS course in Durban, our courses provide the essential training and expertise needed to excel in emergency cardiovascular care.
We continuously strive for excellence in providing high-quality, accredited life support training in the region.
References
- Alshehri, M.F., Pigoga, J.L., & Wallis, L.A. (2020). A mixed methods investigation of emergency communications centre triage in the Government Emergency Medical Services System, Cape Town, South Africa. African Journal of Emergency Medicine, 10(2), 69-75. doi: 10.1016/j.afjem.2020.02.004. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7723918/
- Crause, S., Slabber, H., Theron, E., & Stassen, W. (2023). Telephonic descriptions of out-of-hospital cardiac arrest by laypersons calling the dispatch centre of a private emergency medical service in South Africa. South African Journal of Pre-hospital Emergency Care, 4(1), 2-6. doi:10.24213/4-1-5881. Available at: https://www.journals.ac.za/sajpec/article/view/5881
- Government of South Africa. (2022). Regulations relating to the Standards for Emergency Medical Services, 2022. Government Notice 2819 of 2022. Available at: https://lawlibrary.org.za/akn/za/act/gn/2022/2819/eng@2022-12-02/source.pdf
- Kurz, M.C., Bobrow, B.J., Buckingham, J., Cabanas, J.G., Eisenberg, M., Fromm, P., Panczyk, M.J., Rea, T., Seaman, K., & Vaillancourt, C. (2020). Telecommunicator cardiopulmonary resuscitation: A policy statement from the American Heart Association. Circulation, 141(12), e686-e700. doi: 10.1161/CIR.0000000000000744. Available at: https://www.ahajournals.org/doi/10.1161/CIR.0000000000000744
- Merchant, R.M., Topjian, A.A., Panchal, A.R., Cheng, A., Aziz, K., Berg, K.M., Lavonas, E.J., Magid, D.J., and the Adult Basic and Advanced Life Support, Pediatric Basic and Advanced Life Support, Neonatal Life Support, Resuscitation Education Science, and Systems of Care Writing Groups (2020). Part 1: Executive Summary: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation, 142(suppl 2)–S357. DOI: 10.1161/CIR.0000000000000918. Available at: https://www.ahajournals.org/doi/10.1161/CIR.0000000000000918
- Newton, P.R., Naidoo, R., & Brysiewicz, P. (2015). The appropriateness of emergency medical service responses in the eThekwini district of KwaZulu-Natal, South Africa. South African Medical Journal, 105(10), 844-847. Available at: http://www.samj.org.za/index.php/samj/article/view/9491
- Nolan, J., Schmidbauer, S. & Friberg, H. (2017). Cardiac Arrest Management, Prehospital Care for Cardiac Arrest: How to Improve Outcome. ICU Management practice, 17(2), pages. (80-82) Available at: https://healthmanagement.org/c/icu/IssueArticle/prehospital-care-for-cardiac-arrest-how-to-improve-outcome
- Panchal, A.R., Bartos, J.A., Cabañas, J.G., Donnino, M.W., Drennan, I.R., Hirsch, K.G., Kudenchuk, P.J., Kurz, M.C., Lavonas, E.J., Levy, M.J., Neumar, R.W., Peberdy, M.A., Rittenberger, J.C., Rodriguez, A.J., Sawyer, K.N., Berg, K.M., Chan, P.S., Hazinski, M.F., Morley, P.T., O’Neil, B.J., Soar, J., Travers, A.H., & Yee, T. (2020). Part 3: Adult Basic and Advanced Life Support: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation, 142(suppl 2), S366–S468. DOI: 10.1161/CIR.0000000000000916. Available at: https://www.ahajournals.org/doi/10.1161/CIR.0000000000000916
- South Africa. Department of Health. (2022). Regulations relating to the Standards for Emergency Medical Services, 2022. Government Notice 2819 of 2022, Government Gazette 47632, 2 December. Available at: https://www.gov.za/sites/default/files/gcis_document/202212/47632gon2819.pdf
- South African Human Rights Commission (SAHRC). (2015). Access to Emergency Medical Services in the Eastern Cape. SAHRC Report. Available at: https://www.sahrc.org.za/index.php/sahrc-publications/hearing-reports
- Stassen, W., Wylie, C., Djärv, T., et al. (2021). Out-of-hospital cardiac arrests in the city of Cape Town, South Africa: a retrospective, descriptive analysis of prehospital patient records. BMJ Open, 11, e049141. doi: 10.1136/bmjopen-2021-049141. Available at: https://bmjopen.bmj.com/content/11/8/e049141
- van Rensburg, L., Majiet, N., Geldenhuys, A., King, L.L., & Stassen, W. (2024). A resuscitation systems analysis for South Africa: A narrative review. Resuscitation Plus, 18, 100655. doi: 10.1016/j.resplu.2024.100655. PMID: 38770395; PMCID: PMC11103484. Available at: https://pubmed.ncbi.nlm.nih.gov/38770395/
- Veronese, J.P., Wallis, L., Allgaier, R. and Botha, R., 2018. Cardiopulmonary resuscitation by Emergency Medical Services in South Africa: Barriers to achieving high quality performance. African Journal of Emergency Medicine, 8(1), pp.6-11. DOI: 10.1016/j.afjem.2017.08.005. Available at: https://www.sciencedirect.com/science/article/pii/S2211419X16301872
About the Author
Hi all , I am Ryshane Sewpersad, a seasoned emergency care practitioner with over 15 years of experience across national and international settings. Registered with the Health Professions Council of South Africa and various international bodies, my career spans significant contributions to emergency medical services through course development and the establishment of clinical practice guidelines. My commitment extends to providing quality education and training in the field. An avid adventurer at heart, I am continually in pursuit of new challenges











Responses